COVID-19: IMPACT & NEED FOR PEOPLE WITH DEMENTIA AND FAMILY CARERS
This report produced by The ASI summarises the results of three surveys that were distributed to people living with dementia, family carers, and Community Champions (Understand Together).
The aims of this report are threefold:
- To identify the current challenges experienced by people with dementia and family carers in the current Covid-19 Pandemic through simple surveys.
- To bring together suggestions from people with dementia and family carers of how ASI can continue to support them in lieu of suspended services.
- To communicate the above work in an accessible way to the committee in such a way that will enable the committee to review and shortlist the evidence in a timeline manner.
Results are presented for each individual cohort: People living with dementia, Family Carers, and Community Champions.
PEOPLE LIVING WITH DEMENTIA
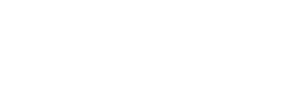
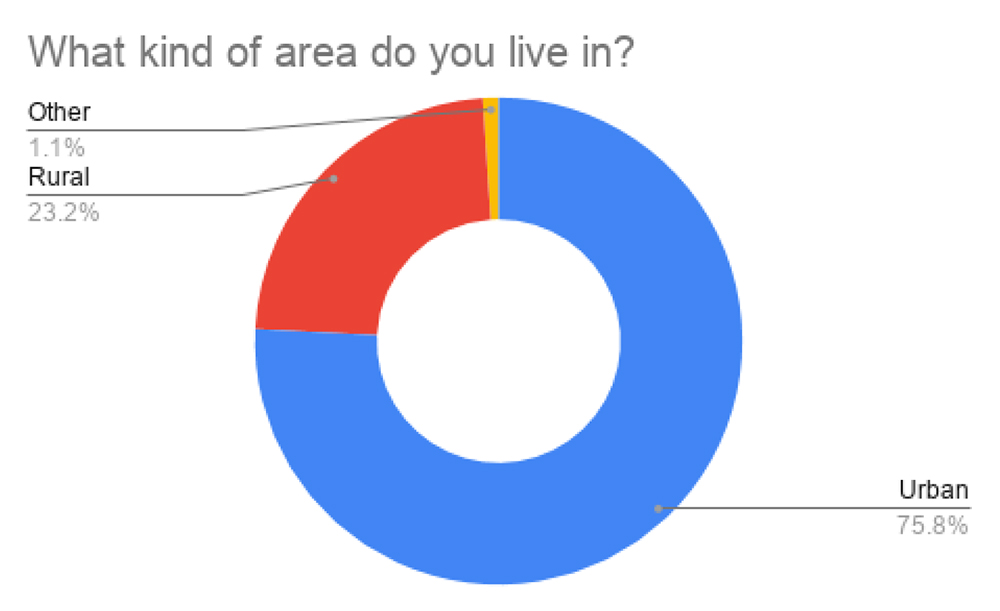
There were 16 responses from people living with dementia. Most of these responses were from members of the Irish Dementia Working Group.
GREATEST CHALLENGES
The below were mentioned by almost every respondent. Loneliness and boredom were mentioned most often and seem to compound respondents’ anxieties.
- Loneliness and Isolation due to social distancing
- Missing daycare services and the socialisation associated with it
- Being housebound is very isolating
- Boredom and lack of routine
- Boredom making it difficult to sleep
- Dementia feels worse being out of usual routine
- Anxiety/Fear
- Unable to purchase supplies independently
- Worried about being on their own and unable to get necessities
- Scared of going shopping and concerned they will forget to keep a social distance
- Concern about accessing healthcare and GP
HELP NEEDED
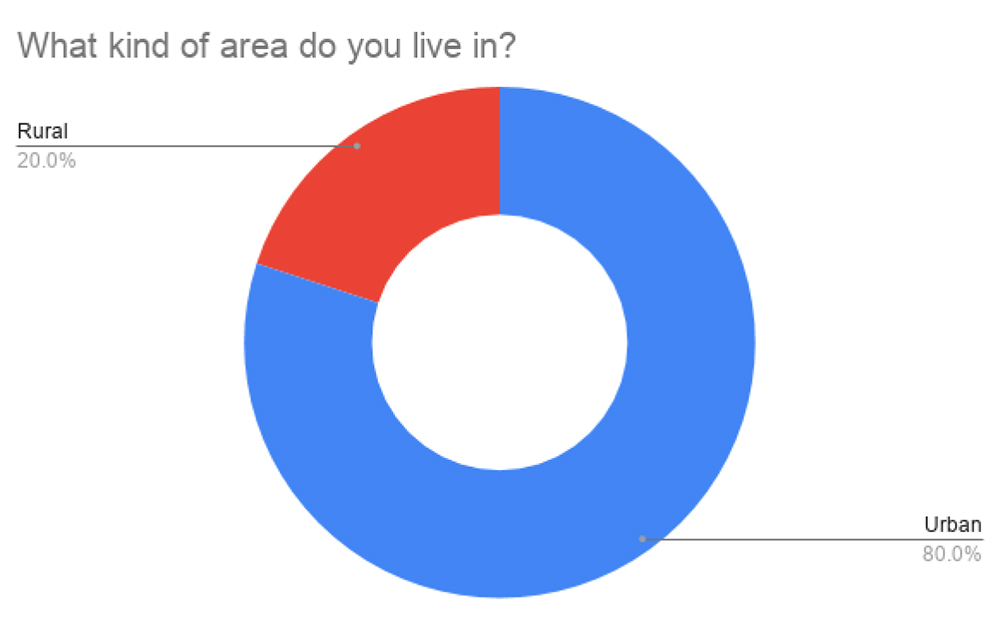
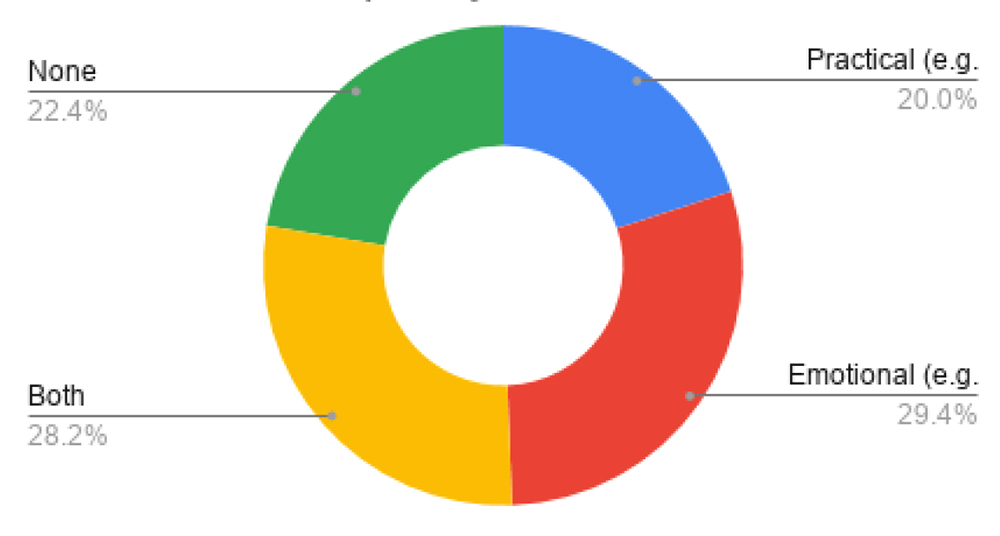
73.3% of respondents feel they need some support at the moment. Most require both practical and emotional supports.
Confidence using ICT
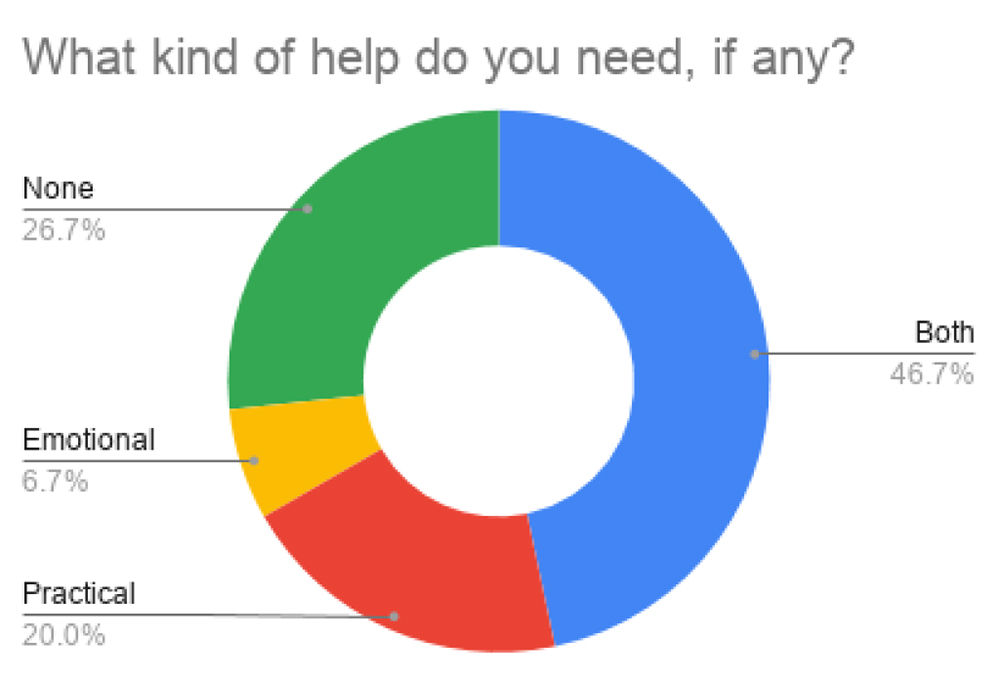
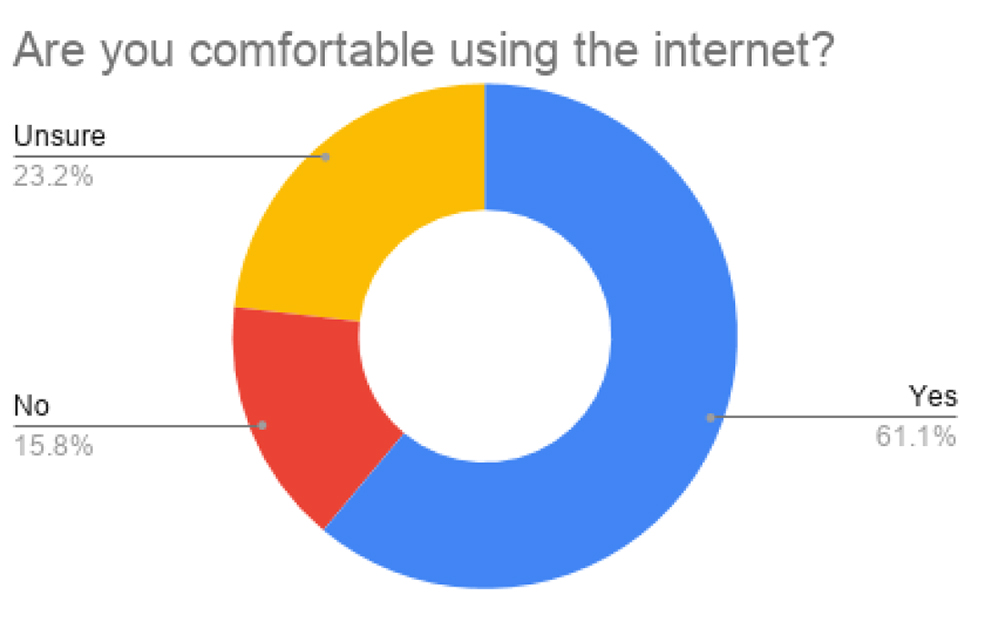
When considering alternative supports, it should be noted that several respondents with dementia are not comfortable using the internet.
While almost one third of this group are comfortable with ICT, they are predominantly younger than the average ASI client and in the earlier stages of dementia.
ALTERNATIVE SUPPORTS
Suggestions were predominantly focused around social and peer support through phone/online contact.
- REGULAR CONTACT FROM ASI: Almost all participants suggested frequent phone calls from an ASI staff member to provide companionship and to ‘check in’ with the person to make sure they are ok.
- PEER SUPPORT FACILITATED BY ASI: Some participants suggested a video call (organised by ASI) with other people affected by dementia for a fun activity and peer support. Three participants also suggested the formation of Whatsapp groups to alleviate loneliness.
- PRACTICAL SUPPORTS: Preparing and delivering meals, collect prescriptions, food shopping, and accompanying people on walks etc (at a social distance)
SUMMARY
The needs of participants living with dementia are centred primarily on alleviating loneliness and isolation.
There is some fear and anxiety that appear to stem from the worry of being ‘forgotten’, boredom, and being unable to purchase necessities independently.
Having ASI ‘check in’ regularly both for companionship and reassurance is a clear need that can help to lessen some of the key challenges experienced by people living with dementia during this time.
FAMILY CARERS
There were 95 responses from Family Carers. Eight of these are family carers who are part of the Dementia Carer Campaign Network. 87 are family carers of day centre clients
GREATEST CHALLENGES
Carers reported on the greatest challenges impacting themselves in addition to the greatest challenges they believe are impacting the person they care for.
Lack of routine for person with dementia leading to responsive behaviours and boredom
For Family Carers
- Fear of not being able to cope with husband’s challenging behaviour for much longer.
- A lack of routine makes it difficult to motivate the PlwD
For person with dementia
- Missing day care and social activities, lack of activity leading to boredom
- Responsive behaviour developing, such as agitation.
Increased anxiety, stress & fear
For family carers
- Anxiety and fear of uncertainty and unknown
- Feeling helpless and smothered by caring work load
- Marked increase in carer burden with little or no support
- Worry about the times when PlwD is alone during the day as there is no service to attend, including library, Church.
- Concern about impact of loss of social interaction for PlwD
- Fear that home care workers might heighten risk of infection even when taking precautions
- Difficult to access healthcare treatment currently
- Worry that PlwD will contract virus and become ill, carers fearful they will become unwell and unavailable to care.
Callers to the ASI Helpline also express concern about delays in response from health care professionals, including GPs and PHNs. It is also reported that people with dementia are being sent home from hospital without adequate home and community support in place.
Among callers to the Helpline, concerns have also been raised about an increase in responsive behaviour due to social isolation and changes in routine.
For person with dementia
- PlwD experiencing distress and upset over loss of care support and social aspects of supports, and as a result, experiencing deterioration of symptoms.
- PlwD is fearful of leaving the house
- Sleep disruption during the night
Being housebound – unable to shop and lack of respite
For Family Carer
- Difficulty getting home help to provide support for PlwD’s personal care
- PlwD is housebound and so carer cannot leave the house, even for a walk.
- Not able to go food shopping, collect prescriptions due to virus
Loneliness & Isolation
For Person with dementia
- PlwD experiencing immense isolation and has no companionship
For Family carer
- Experiencing constant loneliness and feeling trapped at home
- Loneliness and anxious about not being able to see grandchildren, family members
- Feeling abandoned and very fearful, cut off from family and friends
Among callers to the Helplines similar concerns are expressed about the main carer becoming too unwell to care for the person with dementia.
HELP NEEDED
77.6% of family carers reported needing supports at the moment. This includes practical supports (shopping, information etc), emotional supports (e.g. peer support), or both. Almost a quarter 22% felt that they are coping fine for now.
Confidence using ICT
There is a clear need for both online and offline resources given that over one third of family carers sampled do not feel comfortable using the internet or are unsure of it. However, from responses below there is evidently a desire for digital interventions too.
ALTERNATIVE SUPPORTS
Respondents emphasised the need for regular contact and practical help:
- REGULAR CONTACT FROM ASI: This was cited by several family carers. They feel that daily phone calls and a listening ear for the family carer and person with dementia would be really helpful and may alleviate some boredom and worry. Some staff in ASI are currently doing this and there is deep appreciation for it. Family carer looks forward to calls.
- PEER SUPPORT FACILITATED BY ASI: Participants suggested Facetime group meetings or online “buddy” groups, where peers support each other with help from ASI staff members. Some also suggested Whatsapp groups and supportive text messages from others as being helpful.
- ACTIVITIES: Setting daily online challenges that are fun and engaging, including sharing stories. Putting interesting topics online including YouTube videos of activities that would usually take place in the centres and circulate these. Share Spotify list of old music. Give information of TV stations that show old comedy shows & soaps rather than looking at the news.
- RESPITE: Respite for carer, even to take a short walk to get out of the house. This could be an hourlong visit/companionship from ASI staff/ walk with person (at a social distance) by ASI staff members that PlwD knows and is familiar with.
- PRACTICAL SUPPORTS: Help with shopping, collecting prescriptions, dog walking
- INFORMATION: Regular communication and information from ASI and provide information in a way that is accessible, taking into account needs of people who do not access information online
- Continued online family carer training.
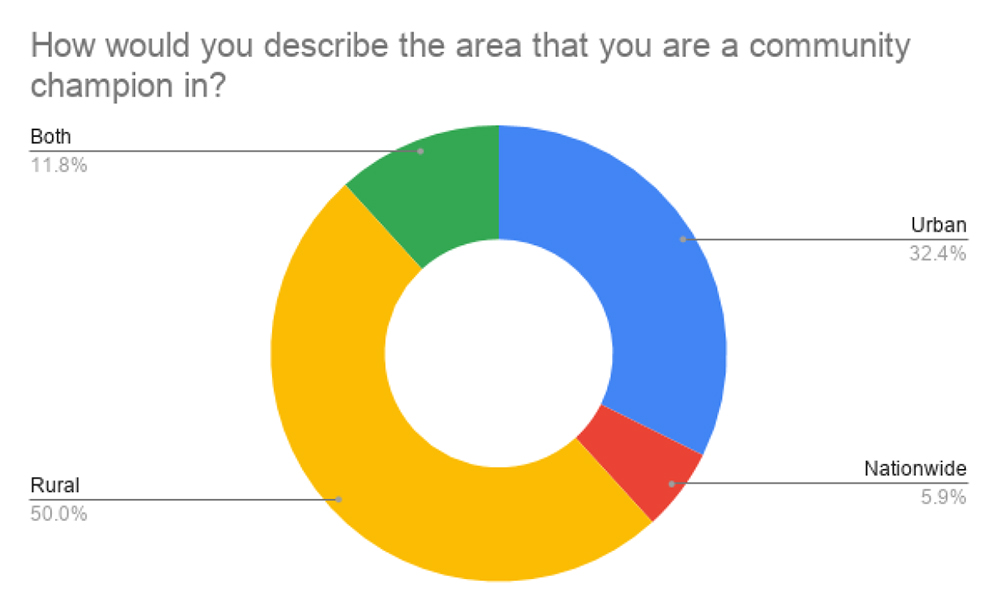
COMMUNITY CHAMPIONS
36 Community Champions responded to the survey. We felt it was important to ask their opinions as they have a sense of what is happening and what are unmet needs in their local community.
GREATEST CHALLENGES
- Loneliness and Isolation:
• Cessation of services leading to lack of routine and reduced opportunity for stimulation and loss of companionship.
• People with dementia living alone are completely isolated - Lack of routine & boredom:
• Reduced engagement opportunities leading to boredom and agitation and responsive behaviour.
• Limited access to accompanied walks and exercise - Anxiety, Fear & Carer Stress:
• Reduced contact with family and other services placing responsibility and pressure on the carers.
• Lack of contact with health / GP services for non-Covid related issues, and anxiety that the needs of PlwD will be overlooked.
• Financial costs and implications for carers
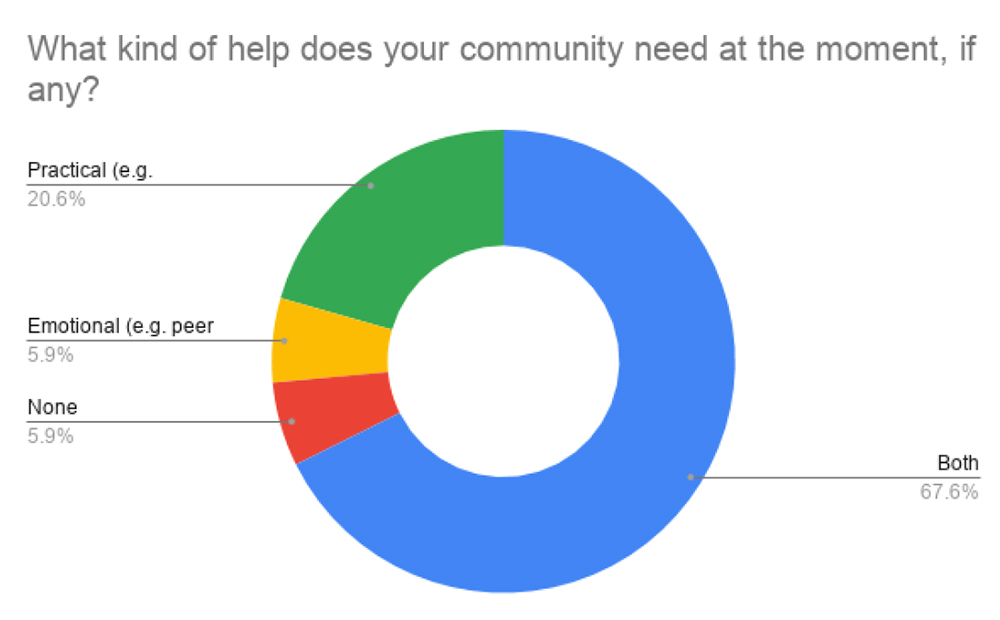
SUPPORT NEEDED
Almost 95% of Community Champions feel that people affected by dementia in their community require either practical or emotional support or both.
ALTERNATIVE SUPPORTS
- Regular Contact from ASI/ Champions: Support calls by phone or skype to PlwD, carers and Champions to circulate information. Phone advice about safety issues, advice about technology.
- Activities: Online activity such as cognitive support, exercise, video about what is happening locally. Interactive online support tool for carers. Day/ weeks plans with ideas for physical and stimulating activities
- Information: Information dissemination, reliable information, also through local radio and newspapers.
- Practical supports: preparing and delivering meals, collect prescriptions, food shopping, dog walking. Spend time with person outside their home- walk, exercise
- Respite: volunteers to allow time out for carers, and support community volunteers
- Befriending on 1:1 basis, individualised support
- Delivering emergency boxes with necessities for people in communities
ALTERNATIVE SUPPORTS ALREADY IN PLACE
Community Champions were also asked if they are aware of any supports for people with dementia and/or family carers that are already happening in their communities
- Aware of ALONE led programme (phone line), but not dementia specific.
- Volunteers from the community collecting and delivering meals to people living alone.
- Garda and sports clubs are offering their services to help older people
- A volunteer network has been set up to help with shopping or to chat.
- Meals on wheels service.
- Volunteer groups in a lot of neighbour hoods but people are fearful about letting strangers in or giving them money to do shopping, need people from a recognised organisation
- General community spirit is in evidence but not aware of any dementia-specific initiatives
DEMENTIA ADVISERS
The DA service has highlighted a number of challenges and concerns facing carers and people living with dementia. These include:
- People who are recently diagnosed and finding it difficult to accept. Family members fear this current impasse is making it difficult to adjust as they cannot engage with services.
- As above, DAs refer to increasing responsive behaviour, including confusion, paranoia, delusions, agitation, and other behavioural changes, with one DA likening deterioration to “falling off a cliff edge”.
- Family carers are struggling to manage responsive behaviour and cannot reply on extended family for support.
- Person with dementia not sleeping at night, and carer experiencing exhaustion and difficulty functioning during the day.
- Family carers are seeking home care support in lieu of normal social activities and services.
- Family members cannot visit the person in hospital or in nursing homes and are concerned that the person is regressing as a result.
- Person with dementia unable to follow hygiene practices, forgetting to wash hands and maintain social distance.
- For people with dementia who are self-isolating, family members fear they will not take medication as prescribed.
- For family members who are living abroad or away from the person with dementia, they is considerable anxiety about how the person will cope.
CONCLUSION:
Participants included 16 people living with dementia and 95 family carers. We also gathered the views of 36 Community Champions who work with people affected by dementia in their local communities. Community Champions reported on how they felt Covid-19 is impacting people with dementia and carers in their community (rather than themselves). Included also are concerns and issues raised by callers to the Helpline and DA service.
Similar challenges were reported across all groups.
These are:
- Loneliness and isolation
- Lack of routine and boredom
- Anxiety/fear
Similarly, all three groups surveyed put forward the same kind of suggestions regarding how ASI can support people affected by dementia. The most popular suggestion was daily phone calls from ASI to people with dementia and carers followed by peer support facilitated by ASI. Respondents expressed appreciate and gratitude for these call, while some emphasised they would like a call from a staff member at the day care centre. For family carers in more difficult circumstances, respite options and information are greatly needed.
There appears to be a place for digital supports (e.g. online activities) in addition to offline supports as approximately 60% of carers and 30% of people with dementia in the survey reported being comfortable using ICT (and having access to the internet).